
After transplant was conclusively ruled out, he was very dispirited. Over the following 9 months, he was under considerable physical and mental stress. This man’s problems started on Crestor (rosuvastatin) and cleared when this was stopped. We considered and screened for all other common conditions and ruled these out. We considered the possibility of a depressive disorder or anxiety disorder but rejected these as explanations for his amnestic episodes. When reviewed 3 weeks later, he reported no further amnestic bouts and was euthymic.

He reported a few days later that he could identify with these so much that he had already discontinued his statin.
#Transient global amnesia lipitor series
I gave him a series of vignettes from Duane Graveline’s Lipitor: The Thief of Memory to read. I raised the possibility of a statin-induced global amnesia. This worried him.Īt this point the coin dropped for me.
#Transient global amnesia lipitor full
In May he came back to my attention when he reported that he was completely unable to remember anything for a full day after his previous dialysis session. Although his HAD depression score rose to 15, I stopped his sertraline in the hope that this would eliminate his rectal bleeding and re-open the possibility of a transplant. In January 2006, he had a further blow – he was being withdrawn from the kidney transplant list owing to the appearance of blood in his faeces. He acknowledged that some of his problems were due to retirement and loss of roles. He scored within the normal range on the hospital anxiety and depression (HAD) scale. He appeared to be adjusting to retirement. But he presented as a man who took pride in his appearance and he was open and co-operative. At this point, he complained that he was lacking direction and losing time – for example, when doing a crossword. In November 2005, after his retirement, the patient was again referred to the liaison service complaining of flashbacks from his military experience after watching a war film. Cognitive function testing showed no abnormality. There was no evidence of neurological abnormality. When trying to work out what was going on, we considered the possibilities of transient ischaemic attacks (mini-strokes) or some metabolic disturbance as possible triggers for these episodes. This made him very unhappy but when I interviewed him he did not appear to depressed or psychotic. He was later obliged to retire against his wishes on ill-health grounds. He complained of feeling disorganized at these times. In September, the man’s wife reported that he was having episodes when he was uncertain where he was or what he was supposed to be doing. There was no evidence that he was psychotic or delirious. But he described feeling that there were further episodes happening for which he had no recall. They referred him to me. He didn’t seem remotely depressed and denied any thoughts of self-harm. The renal physicians apparently knew what was going on – this incident and concerns that he might be drinking more water than advised led them to think he was trying to commit suicide. He vaguely remembered freeing himself from the lines and retiring to bed. In the other, during home dialysis he had cut the lines into the dialysis machine with a pair of scissors. In one, he made 40 cups of tea but could later give no reason for this other than he must have been dreaming of having guests to the house. In February, two bizarre episodes happened. At this point the medical notes contain no mention of confusion.
On Crestor his cholesterol level dropped to 3.0 mmol/L. Prior to the change to Crestor, his cholesterol level had tracked at a healthy 4.5 mmol/L but had jumped to 6.3 mmol/L (lower than mine).
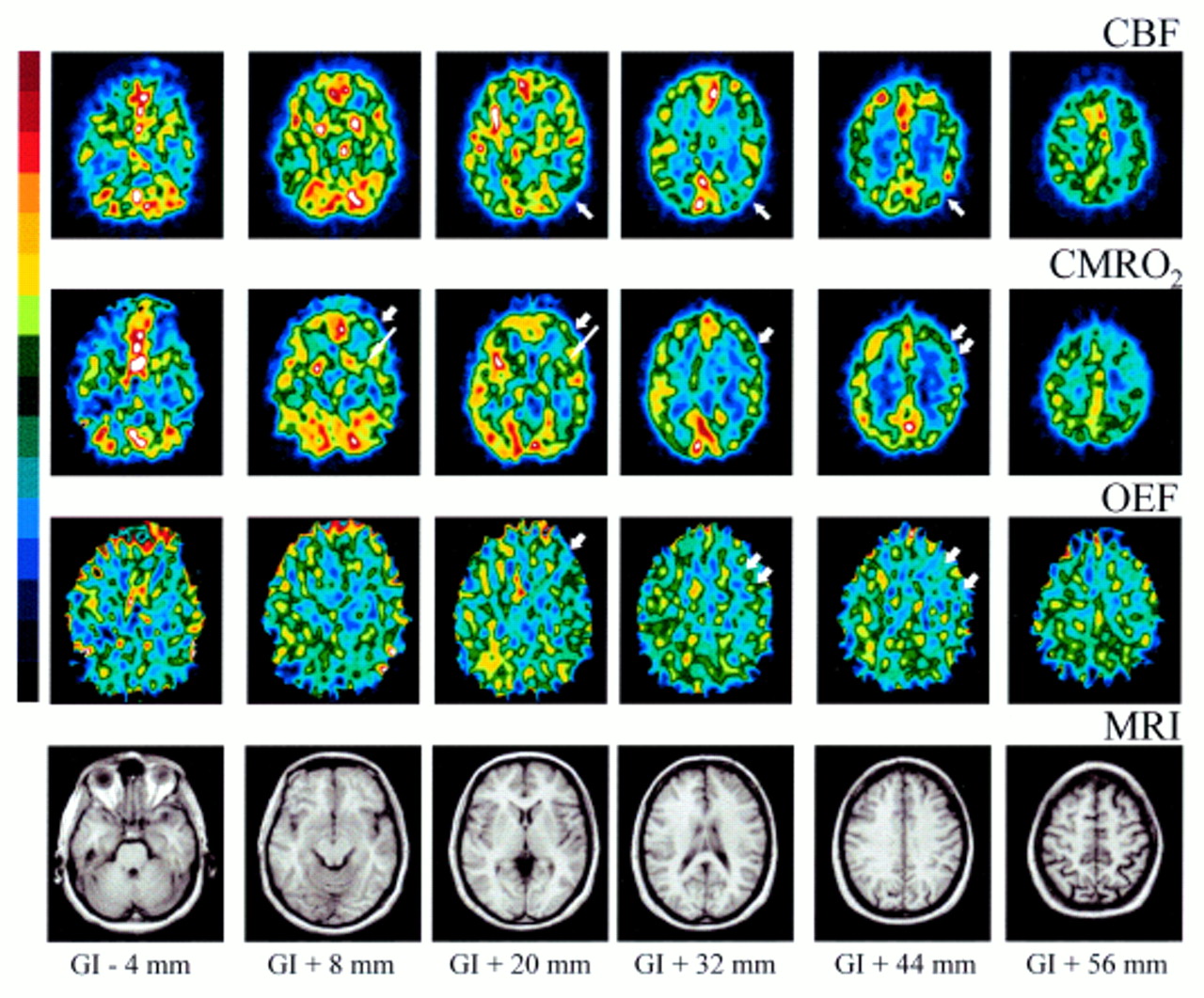
His Zocor was changed to 10 mg rosuvastatin – Crestor. His primary care doctor prescribed an antidepressant, dosulepin, but later changing this to sertraline – Zoloft. Over time he got physically worse and got more distressed. At this point he was on medication for blood pressure and was begun on 40 mg of simvastatin – Zocor. He was started on dialysis for his renal failure. In 2001, a 57-year-old man presented to hospital with end-stage renal failure secondary to kidney disease. This case has already appeared in BMJ – see below – but with no effect. Many people might ask why post a story like this here and court media attention – this is a scientific issue to be dealt with in journals. This one deals with one of the more complex problems these drugs can cause – cognitive failure.

The first two were Birth of a Statinista and The Legacy Effects of Statins. Editorial Note: This is a third post on Statins.


 0 kommentar(er)
0 kommentar(er)
